Abstract
The immune system plays a crucial role in maintaining the health and protection of the human body against microbial invasions. However, this same system can lead to exaggerated immune and inflammatory responses resulting in adverse outcomes known as hypersensitivity reactions. There are four traditional classifications for hypersensitivity reactions, and these include type I, type II, type III, and type IV reactions:
IgE Mediated (Type I) Hypersensitivity is also known as an immediate reaction and involves immunoglobulin E (IgE)-mediated release of antibodies against the soluble antigen. This results in mast cell degranulation and the release of histamine and other inflammatory mediators.
Type II hypersensitivity is also known as cytotoxic reactions and involves IgG and IgM antibodies, leading to activation of the complement system and cell damage or lysis.
Type III hypersensitivity is also known as immune complex reactions and involves IgG, IgM, and sometimes IgA antibodies. Accumulation of these immune complexes results in inactivation of the complement system, leading to chemotaxis of polymorphonuclear leukocytes (PMNs) and ultimately causing tissue damage.
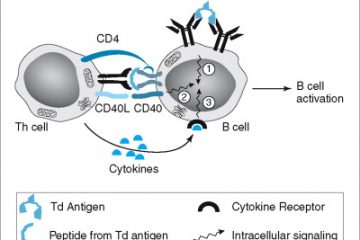
Type IV hypersensitivity is also known as delayed-type and involves T cell-mediated reactions. T cells or macrophages become activated as a result of cytokine release, leading to tissue damage.
There has been a more recent classification introduced by Sell et al. which accounts for multiple components of the immune system and classifies reactions into seven parts. However, the focus of this article will be on the classic Type I hypersensitivity reactions.
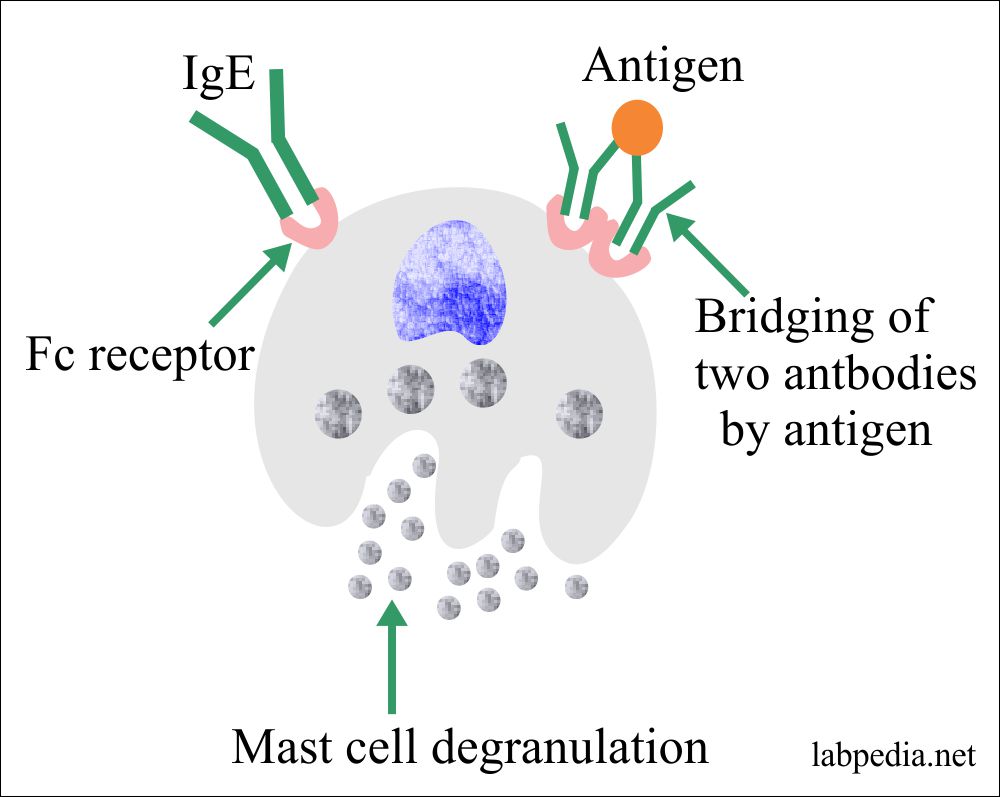
Type I hypersensitivities include atopic diseases, which are exaggerated IgE-mediated immune responses (i.e., allergic: asthma, rhinitis, conjunctivitis, and dermatitis), and allergic diseases, which are immune responses to foreign allergens (i.e., anaphylaxis, urticaria, angioedema, food and drug allergies). The allergens that cause type I hypersensitivity can be harmless (ie pollen, dust mites, food, medication, etc.) or more dangerous, such as insect poisons. The reaction can manifest itself in different areas of the body and can result in cases such as:
- Nasal allergic rhinitis or hay fever
- Allergic ocular conjunctivitis, possibly due to seasonal allergens such as pollen or mould spores
- Dermatologic urticaria, atopic eczema, or erythema
- Soft tissue angioedema
- Pulmonary reactions, such as allergic asthma or hypoxia.
- A systemic reaction is a life-threatening medical emergency and also known as anaphylaxis.
There are certain risk factors that increase the risk of allergic diseases. These factors include geographic distribution, environmental risks such as pollution or socioeconomic status, genetic predisposition, or the “hygiene hypothesis.” The “hygiene hypothesis” suggests that the good hygiene practices of our modern society and the lack of early exposure to many microbes or antigens can lead to the failure of the immune system to function. As such, the hypothesis suggests that early exposure to a wide range of microorganisms and antigens may actually lead to overall lower rates of allergies, asthma, and other immune disorders.